Others
Protocols
Normal level :
- 1 to 16 years = 51 to 217 pg/mL
- Adult = 50 to 300 pg/mL
Increased PTH Level Is Seen In:
- Primary hyperparathyroidism.
- Pseudohypoparathyroidism ( Secondary hyperparathyroidism ).
- Vit. D deficiency ( hereditary ) and rickets.
- Zollinger Ellison syndrome.
- Non-PTH producing tumors give rise to the paraneoplastic syndrome,
- Chronic renal failure.
- Hypocalcemia.
- Malabsorption.
Decreased PTH Level Is Seen In:
- Grave’s disease ( Hypoparathyroidism ).
- Non-Parathyroid hypercalcemia.
- Surgical, secondary hypoparathyroidism.
- Sarcoidosis.
- Metastatic bone tumors.
- Vit.D intoxication.
- Milk-alkali syndrome.
- DiGeorge syndrome.
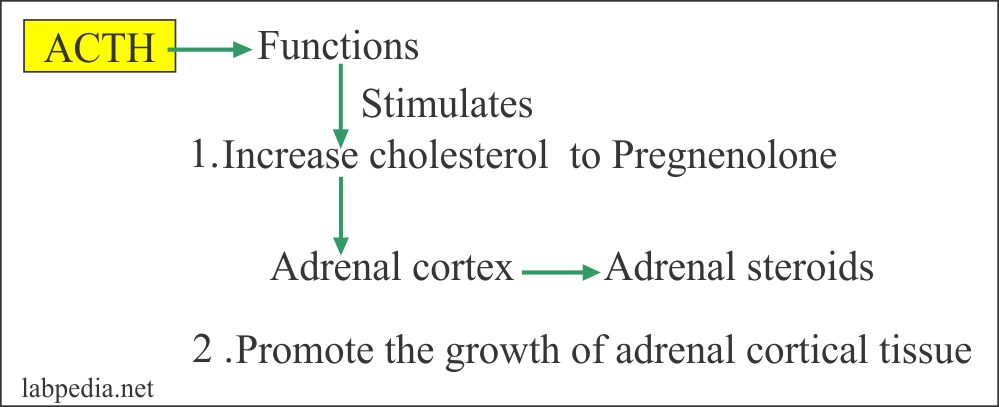
Adrenocorticotropic hormone(ACTH)
- This is a polypeptide hormone produced by the corticotropic cells of the anterior pituitary gland.
- ACTH is a tropic hormone, it binds to the cells of the adrenal cortex and influences their activities.
- ACTH in plasma is highest between 6 to 8 AM and lowest in the evening between 6 to 11 PM.ACTH action on adrenal cortex
- ACTH may be raised as primary or ectopic production.
- Ectopic production from:
- Small cell carcinoma of the lung ( >200 ng/L).
- Pancreatic carcinoma.
- Breast.
- Stomach.
- Colon.
- Benign conditions are:
- Chronic obstructive pulmonary disease.
- Mental depression.
- Obesity.
- Hypertension.
- Diabetes.
- Stress.
- ACTH in normal person does not exceed 50 pg/mL at its peak and the basal level is near 5 pg/mL.
- Raised ACTH level is seen in:
- In primary adrenal deficiency.
- In patients with Cushing’s syndrome.
- In patients with ectopic tumors e.g.
- Basophilic neoplasm of the anterior pituitary.
- Ectopic carcinoma of the lung.
- Normal
- AM level = <80 pg/mL (<18 pmol/L).
- PM level = <50 pg/mL (<11 pmol/L).
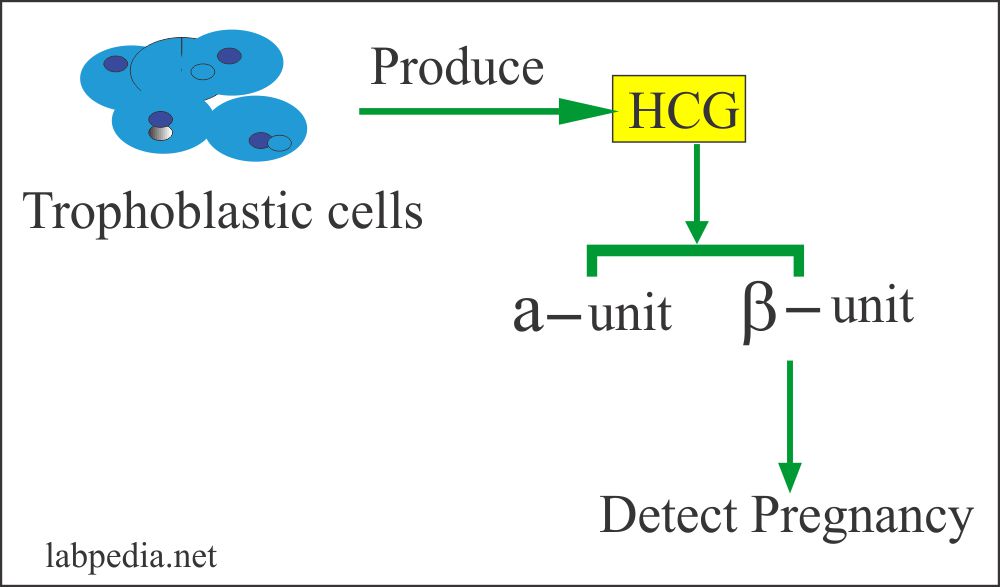
Human Chorionic gonadotropin hormone (HCG)
- This is also called Chorionic gonadotropin.
- This is a glycoprotein secreted by the syncytiotrophoblastic cells of the placenta.
- This consists of two subunits:
- α- HCG.
- β-HCG.
- This consists of two subunits:
- Elevated HCG level is seen in:
- Trophoblastic disease (level is usually >one million IU/L).
- Germ cell tumor and non-seminomatous tumors of the testis (there is a moderate increase).
- Reported in melanoma and carcinoma of the breast, GIT tumors, lung, and ovary.
- The presence of HCG in seminoma indicates another component as choriocarcinoma.
- Also raised in benign conditions like:
- Cirrhosis.
- Duodenal ulcer.
- Inflammatory bowel diseases.
- Pregnancy.
- Normal HCG
- Male and nonpregnant females = <5 mIU/mL.
Calcitonin
- This is a polypeptide with 32 amino acids.
- This is produced by the C cells of the thyroid.
- The serum half-life is 12 minutes.
- In a normal person is <0.1 µg /L.
- This is produced in response to increased serum calcium levels.
- Calcitonin is useful for the monitoring of disease after treatment.
- It inhibits the release of calcium from the bone, lowers the serum calcium.
- Calcitonin is useful to diagnose :
- Medullary carcinoma of the thyroid.
- Carcinoid tumor.
- Lung cancers.
- Breast cancer.
- Kidney tumor.
- Liver tumor.
- Calcitonin level also raised in nonmalignant conditions like:
- Pulmonary disease.
- Pancreatitis.
- Hyperparathyroidism.
- Paget’s disease of bone.
- Pregnancy.
- Pernicious anemia.
- Normal (Source 2)
- Basal (plasma)
- Male = ≤19 pg/mL (≤19 ng/L)
- Female = ≤14 pg/mL (≤14 ng/L)
- Calcium infusion (2.4 mg/kg)
- Male = ≤190 pg/mL (≤190 ng/L)
- Femal = ≤130 pg/mL (≤130 ng/L)
- Pentagastrin injection (0.5 µg/kg)
- Male = ≤110 pg/mL (≤110 ng/L)
- Female = ≤30 pg/mL (≤30 ng/L)
- Basal (plasma)
Normal level:
Women before puberty = 0 to 4 mIU/L
- Menstruating women
- Follicular = 5 to 20 IU/L.
- Ovulatory phase = 30 to 50 IU/L.
- Luteal phase = 1.09 to 9.2 IU/L.
- Women post menopause = 19.5 to 100.6. IU/L.
- Men before puberty = 0 to 5 mIU/L
- Men during puberty = 1.42 to 15.4. IU/L
- Men adult = 1.5 to 12.5 IU/L.
- Children:
- Male = 0.3 to 4.6 IU/L.
- Female = 0.68 to 6.7 IU/L.
High FSH:
- Loss of ovarian function before age 40 (ovarian failure).
- Polycystic ovary syndrome (PCOS).
- Menopause has occurred.
- Pituitary adenoma.
- Precocious puberty.
- Ovarian dysgenesis ( Turner syndrome ).
High FSH values in a man:
- Klinefelter syndrome ( Testicular dysgenesis ).
- Testicles are absent or not functioning properly.
- Testicles have been damaged by alcohol dependence or treatments like X-rays or chemotherapy.
- High values in children may mean that puberty is about to start.
- Complete testicular feminization syndrome.
Decreased FSH :
- Pituitary failure.
- Hypothalamic failure.
- Stress.
- Anorexia nervosa.
- Malnutrition.
Low Values Of FSH Indicate:
- A woman not producing eggs (prevents ovulation) leads to infertility.
- A man is not producing sperm.
- The hypothalamus or pituitary gland is not functioning properly.
- A tumor is present that interferes with the brain’s ability to control FSH production.
- Stress.
- Starvation or being very underweight.
Normal Level:
| IU/L | ||
| Male | 1.24 to 7.8 | |
| Female | ||
| Follicular | 1.6 to 15 | |
| Ovulatory phase | 21.9 to 56.6 | |
| Luteal phase | 0.61 to 16.3 | |
| Postmenopausal | 14.2 to 52.3 | |
| Child | Male 1 to 10 years | 0.04 to 3.6 |
| Female 1 to 10 years | 0.03 to 3.9 |
Increased values of (LH) :
- A gonadal failure like:
- Menopause.
- Ovarian dysgenesis. (Turner syndrome).
- Testicular dysgenesis (Klinefelter syndrome).
- Precocious puberty.
- Pituitary adenoma.
- Raised level of both LH and FSH is seen in:
- Gonadal failure.
- Polycystic ovary.
- During menopause.
Decreased values of LH:
- Pituitary failure. Both LH/ FSH are low.
- Hypothalamic failure will also lead to low LH and FSH levels.
- Stress.
- Anorexia nervosa.
- Malnutrition.
- In secondary gonadal failure, the LH and FSH level is low.
Normal level:
Total Testosterone
- Men = 3 to 10 ng/mL
- Women = <1 ng/mL
- Prepubertal boys and girls = 0.05 to 0.2 ng/mL
Free testosterone
- Men = 50 to 210 pg/mL.
- Women = 1.0 to 8.5 pg/mL.
- Children:
- Boy = 0.1 to 3.2 pg/mL.
- Children Girl = 0.1 to 0.9 pg/mL.
- Puberty:
- Boy = 1.4 to 156 pg/mL.
- Puberty Girls = 1.0 to 5.2 pg/ml.
Total Testosterone
- Men = 270 to 1070 ng/dL.
- Women = 15 to 70 ng/dL.
- Postmenopausal women = 8 to 35 ng/dL.
- Pregnant women = 3 to 4 ng/dL
Increased Values Of Total Testosterone :
- Male
- hyperthyroidism.
- Adrenal tumors.
- Adrenal Hyperplasia.
- Hypothalamic tumor, Pinealoma.
- Viral encephalitis.
- Testicular or extragonadal tumors where Leydig cells produce testosterone.
- Testosterone resistance syndrome.
- Female
- Adrenal neoplasm.
- Hilar cell tumor.
- Idiopathic Hirsutism.
- Trophoblastic disease during pregnancy
- Ovarian tumors
- Polycystic ovary.
Decreased Total Testosterone Value In Male:
- Klinefelter syndrome.
- Pituitary failure leading to hypogonadism.
- Hypopituitarism may be primary or secondary.
- Orchiectomy.
- Delayed puberty.
- Down syndrome (trisomy 21).
- Cirrhosis.
- Cryptorchidism due to undescended testes.
Increased Free Testosterone in Female:
- Hirsutism.
- Virilization.
- polycystic ovaries.
Decreased Free Testosterone Is Seen In Male:
- Hypogonadism.
- old age.
Normal level;
- Adult male = 0 to 20 ng/mL
- Adult female = 0 to 25 ng/mL
- Pregnant female = 20 to 400 ng/mL
1.Increased prolactin
level is seen in :
- Breast
stimulation.
- Pregnancy.
- Nursing.
- Stress.
- Exercise.
2.Pituitary tumors form
acidophilic cells that produce prolactin.
3.The moderate level
increase is seen in :
- Secondary
amenorrhea.
- Galactorrhea.
- primary
hypothyroidism.
- Polycystic ovary syndrome.
Decreased Prolactin Level Is Seen In:
- Sheehan’s syndrome (after delivery may have hemorrhage or infarction of the pituitary gland).
- Pituitary destruction by the tumors e.g. Craniopharyngioma.
Hyperprolactinemia Leads To In:
- Females
- Anovulation With or without irregularity in menstruation.
- Galactorrhea and amenorrhea.
- Or galactorrhea alone.
- In Males
- Oligospermia
- May have impotence.
- Or both.
- 30% of the microadenoma patients have a clinically silent tumor. But the PRL level will be raised.
- Imaging like CT or MRI is advised.
- Patients with >150 ng/mL have PRL secreting tumors.
- Many patients have >1000 ng/mL of PRL.
- PRL level >200 ng/mL is enough evidence for PRL-secreting pituitary tumors.