Urine R/M/E
Protocols
Urine normal values are:
| Urine substances to be checked | Normal values | Collection timings | Significance |
| Physical characteristics | |||
|
| A random and fresh sample |
|
| Variable, pale-yellow to dark amber | A random sample | Red color urine, check for hemoglobin |
| Faint aromatic | A random sample | Urine from a diabetic patient has a fruity (acetone) odor. |
|
|
|
|
|
|
|
|
|
|
|
|
| Chemical characteristics | |||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
|
| 24 hours urine sample | It is part of the acid-base balance. |
|
| 24 hours urine sample | |
|
| 24 hours urine sample | |
|
|
| |
| 0 to 3 mg/day | 24 hours urine sample | |
| 10 to 35 g (average 15 g) | 24 hours urine sample | |
|
| 24 hours urine sample | |
|
| 24 hours urine sample | |
|
| ||
|
|
| |
|
|
| |
| 0.5 to 2.2 g (average 1.0 g) | 24 hours urine sample | |
|
| 24 hours urine sample | |
|
| 24 hours urine sample | |
|
| A random sample (Check within one hour) |
|
|
|
|
|
|
|
|
|
|
|
|
|
| Negative | A random sample | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| 24 hours urine sample |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
| Microscopic characteristics | |||
|
| A random sample | The persistent presence of RBCs in the urine needs thorough investigations |
| 0/HPF | A random sample | Indicates hemorrhage in the nephron |
|
| A random sample | Urine culture should be done when increased WBCs are found |
| Negative | A random urine sample | Seen in renal inflammatory diseases |
|
| A random sample | |
| Occasional 0 to 2/HPF | A random sample | Usually seen when there is damage to the glomerular capillary membrane |
| Occasional 0 to 2/HPF | A random sample | These indicate renal disease |
| Negative | A random sample | In renal failure (severe renal disease) |
| Negative | A random urine sample | Seen in diabetic nephropathy |
| Absent | A random urine sample | UTI due to Trichomonas vaginalis |
| Absent | A random urine sample | Genitourinary infection |
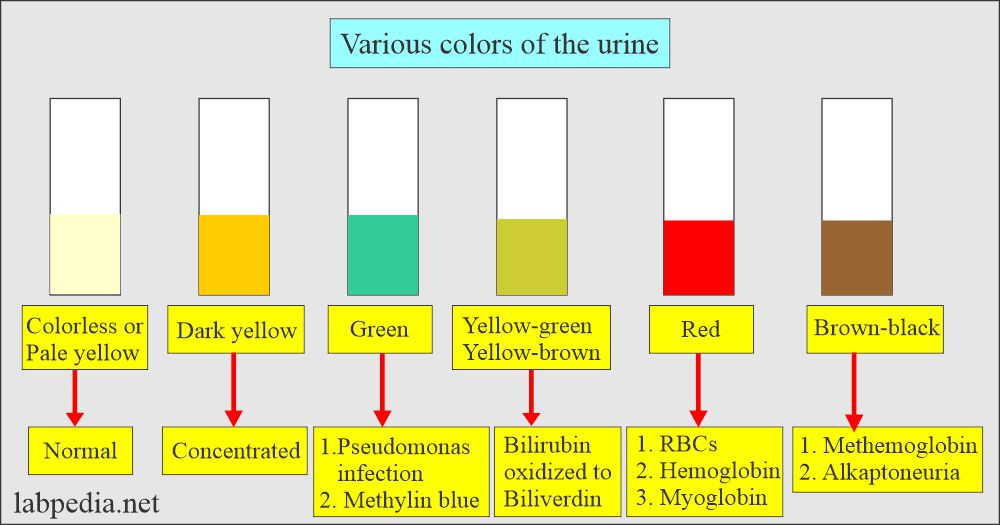
Urine Color :
| Urine color | Pathological causes | Nonpathological causes |
| Red or reddish-brown |
|
|
| Green |
|
|
| Blue or blue-green |
|
|
| Orange |
|
|
| Yellow-orange or yellow-brown |
|
|
| Black or brownish-black |
|
|
| Milky or opalescent |
|
Drugs that can change the color of the urine:
| Drugs | Effect of the drug on the body | Change in the urine color |
| Chloroquine | Antimalarial drug | Rusty yellow or brown |
| Iron preparation | Treat the anemia | Drak brown and becomes black on standing |
| Nitrofurantoin | Antibacterial for UTI | Brown |
| Pyridium (Phenazopyridine) | Urinary tract analgesic | orange to red |
| Dilantin | Anticonvulsant for epilepsy | Pink, red, or red-brown |
| Vitamin B 2 (Riboflavin) | Vitamin supplement | Dark yellow |
| Levodopa | Treat Parkinson’s disease | Dark-brown on standing |
| Rifampicin | Antibacterial for TB | Red-orange |
| Dyrenium ( Triamterene) | Diuretic | Pale-blue |
| Cascara sagrada | Laxative | Red in alkaline urine and yellow-brown in acidic urine |
| Doxidan (Docusate calcium) | Laxative | Pink to red to red-brown |
| Phenolphthalein | Laxative | Red or purplish-pink in alkaline urine |
| Phenothiazine | Antiemetic, antipsychotic, neuroleptic | Red-brown |
| Sulfasalazine | Antibacterial | Orange-yellow in alkaline urine |
Various odors of the urine:
| Odor | The reason for that odor |
| Faint aromatic (fresh urine) | Due to ammonia |
| Strong, unpleasant odor | Bacterial infection |
| Sweety or fruity odor | Diabetes mellitus ketone bodies |
| Maple syrup odor | Maple syrup disease |
| Unusual pungent odor | Ingestion of onions, garlic, and asparagus |
| Mousy odor | Phenylketonuria |
| Sweet smell | Malnutrition, vomiting, and diarrhea |
Urine clarity variables:
| Urine degree of clarity (cloudiness) | Criteria |
| Clear |
|
| Hazy |
|
| Cloudy |
|
| Turbid |
|
Normal urine specific gravity :
- 1.003 to 1.030 (1.005 to 1.030).
- Most urine fall in the range of 1.015 to 1.025.
- Newborn = 1.012
- Infants = 1.002 to 1.006
- Adult = 1.002 to 1.030
- After 12 hours of fluid restriction = >1.025
- Urine 24 hours = 1.015 to 1.025
- The diluted urine range is 1.000 to 1.010.
- Concentrated urine is 1.025 to 1.030.
Low specific gravity urine (hyposthenuria) is seen in:
- Diabetes inspidus (not go above 1.001 to 1.003. ADH hormone is lacking.
- Pyelonephritis.
- Glomerulonephritis.
- The consistent low specific gravity of 1.010 is known as isosthenuria.
- It is seen in chronic renal disease, where the capacity of concentrating urine is lost.
High specific gravity urine (hypersthenuria) is seen in:
- Diabetes mellitus.
- Congestive heart failure.
- Dehydration due to sweating, fever, and vomiting or diarrhea.
- Adrenal insufficiency.
- Liver disease.Nephrosis.
Causes of acidic and alkaline urine:
| Alkaline urine (pH is alkaline) | Acidic urine (pH is acidic) |
|
|
- Normal:
- 500 to 800 mOsm/ kg of water.
- Serum osmolarity = 275 to 300 mOsm.
- Urine osmolarity = 50 to 1400 mOsm.
- Use of the osmolality/osmolarity:
- It can monitor renal concentration ability for the course of renal disease.
- It can monitor fluid and electrolyte therapy.
- It can differentiate between hypernatremia and hyponatremia.
- It evaluates the secretion and renal response to ADH.
- There is a need to get the osmolarity of the serum and the urine.
- Normal:
- 1200 to 1500 mL/24 hours.
- The range of 600 to 2000 mL/24 hours may be considered normal.
- The average urine volume is 1200 ml.
- Night urine volume is usually less in amount.
- The ratio of day urine to night’s urine is 2: 1 to 4:1.
- 2.Nocturnal polyuria:
- There is increased urine at night. This may be seen in diabetes mellitus and diabetes inspidus.
- This may be seen as diuretics, or intake of tea, coffee, or alcohol. These will suppress the ADH.
- Polyuria is seen in:
- diabetes mellitus.
- Diabetes inspidus.
- Chronic renal disease.
- In the case of acromegaly.
- In the case of myxedema.
- Oliguria:
- There is a decrease in the normal daily urine volume.
- Anuria or oliguria, where urine volume is <200 mL/day.
- This is seen in dehydration due to vomiting, diarrhea, perspiration, or severe burn.
- Nephritis.
- Urinary tract obstruction.
- Acute renal failure.
- Oliguria may lead to anuria.
- Drugs that have diuretic effects are:
- Thiazides.
- Alcohol.
- Caffeine.
- The drugs which decrease the volume and are nephrotoxic are:
- Analgesics like salicylates.
- Antibiotics like neomycin, penicillin, and streptomycin.
- There is a decrease in the normal daily urine volume.
Clinical types of proteinuria are:
Prerenal proteinuria:
- This is caused by nonrenal diseases and is transient; it is seen in:
- Hemoglobinuria.
- Myoglobinuria.
- Acute phase proteinuria.
- This is usually not detected by the routine urine reagent strips.
Renal proteinuria:
- This is due to renal diseases involving glomeruli or tubules.
- Albumin appears in the urine in glomerular damage, followed by the WBCs and RBCs.
- It is seen in:
- SLE.
- Streptococcal glomerulonephritis.
- Strenuous exercise (reversible condition).
- Pre-eclampsia and hypertension. (reversible condition).
- Toxic heavy metals.
- Severe viral infection.
Postrenal proteinuria:
- Proteins can be added as the urine passes through the ureter, urinary bladder, and urethra.
- Bacterial and fungal infection of the lower urinary tract,
- Menstrual contamination also contains proteins.
- Prostatic fluid and spermatozoa.
Orthostatic or postural proteinuria:
- This is a persistent benign condition frequently seen in young patients.
- It appears when the person is upright and disappears when the patient lies down.
- Procedure to confirm the diagnosis:
- These patients are advised to empty their bladder before going to bed.
- Take the first urine sample when patients get up.
- Take another sample when patients are upright for several hours.
- The first sample will be negative.
- The second sample will be positive in orthostatic proteinuria.
Type and degree of proteinuria:
| Degree of proteinuria | Amount of protein excreted in the urine | Etiology |
|
|
|
|
|
|
|
| 1. Chronic pyelonephritis 2. Polycystic kidneys 3. Renal tubular diseases
|
|
| Occurs only when the patient is standing or walking |
|
|
|
Renal glycosuria:
- It is seen when the blood glucose level is normal and glucose appears in the urine.
- Renal tubules’ absorption of glucose by the tubules is compromised.
- It is usually seen in end-stage kidney diseases, osteomalacia, and Fanconi’s syndrome.
- Glucose false tests are seen in the urine’s high specific gravity and contain a large amount of ascorbic acid.
Hyperglycemia of nondiabetic origin is seen in:
- It is seen in the following conditions:
- Pancreatitis.
- Pancreatic cancer.
- Acromegaly.
- Cushing’s syndrome.
- Hyperthyroidism.
- Pheochromocytoma.
- The above conditions produce hormones like glucagon, epinephrine, cortisol, thyroxine, and growth hormone.
- These hormone acts against insulin and leads to glycogenolysis.
Indications for the ketone bodies:
- Diabetic acidosis.
- Starvation.
- Vomiting.
- Malabsorption syndrome.
- Pancreatic disorders.
- Insulin dosage monitoring.
- Strenuous exercise.
- Inborn error of amino acid metabolism.
Ketones are the intermediate products of fat metabolism, and these are:
- acetone.
- Acetoacetate.
- β-hydroxybutyric acid.
Indications for urobilinogen in the urine:
- Early detection of liver diseases.
- Hemolytic diseases.
- Hepatitis and Cirrhosis.
- In carcinomas.
Increased level of urobilinogen is seen in:
- Hemolytic anemia.
- Pernicious (megaloblstic) anemia.
- Malarial attack.
- Excessive bruising.
- Pulmonary infarction.
- Cirrhosis.
- Acute hepatitis.
- Cholangitis.
A decreased level of urobilinogen is seen in:
- Complete or partial obstruction of the biliary tract.
- Cholelithiasis.
- Biliary duct inflammation.
- Cancer of the head of the pancreas.
- Antibiotic therapy will suppress intestinal bacterial flora.
Normal bilirubin level in urine:
- Urine bilirubin is negative (0 to 0.2 mg/dL (0 to 0.34 µmol/L).
- Bilirubin can be detected in urine by the Foam test.
- Increased bilirubin in the urine is seen in:
- Hepatitis and liver diseases.
- Obstructive biliary tract disease.
- Liver or biliary tract tumors.
- Septicemia.
- Hyperthyroidism.
- Hemoglobinuria causes are:
- It may result from the hemolysis of RBCs in the urinary tract. This happens in the dilute and alkaline urine.
- This can also occur in intravascular hemolysis, where hemoglobin filters out through the glomeruli. No RBCs will be seen in the urine.
- Pathogenesis:
- Under normal conditions, the complex of hemoglobin+haptoglobin complex can not filter out of the glomeruli.
- This happens when the free hemoglobin exceeds the haptoglobin e.g.
- Hemolytic anemia.
- Transfusion reactions.
- Infection.
- Severe burns.
- Strenuous exercise.
- Malarial infection.
- Causes are:
- Crush syndrome.
- Muscle wasting diseases.
- Trauma.
- Alcoholism.
- Convulsion.
- Extensive exertion.
- Heroin abuse.
Normal phosphorus in urine:
- Serum level = 2.4 to 4.1 mg/dL (0.78 to 1.34 mmol/L).
- Urine = 1 gram / 24 hours.
- This also depends on the diet.
- Inorganic phosphate = 20 to 40 meq/L.
- Indication for urinary 24 hours phosphorus:
- In hyperparathyroidism.
- In hypoparathyroidism.
- In case of renal losses.
Normal creatinine in urine:
- 1.0 to 1.6 gm/24 hours.
- Or 15 to 25 mg/ kg body weight / 24 hours.
- Indications:
- To evaluate kidney diseases.
- Indications:
- Cystitis.
- Pyelonephritis.
- Monitoring of the patients who are at high risk for urinary tract infection.
- Monitoring of antibiotic therapy.
- Screening of the urine culture specimens.
- Indication for urinary sodium:
- Electrolytes imbalance.
- Acute renal failure.
- Hyponatremia.
- Oliguria.
- Na+ excreted for diagnosis of renal and adrenal imbalance. No preservative is needed for the collection for 24 hours ; only refrigerate during the collection.
- Increased sodium in urine is seen in:
- Addison’s disease (adrenal failure, primary and secondary).
- Renal tubular acidosis.
- Diabetic acidosis.
- Tubulointerstitial disease.
- Salt losing nephritis.
- Barrter’s syndrome
- A decrease in urinary sodium is seen in:
- Excessive sweating and diarrhea.
- Prerenal azotemia.
- Cushing’s syndrome.
- Primary aldosteronism.
- Congestive heart failure.
- Nephrotic syndrome with acute oliguria.
Normal potassium in urine:
- Adult = 25 to 125 meq/24 hours urine (25 to 125 mmol/day).
- Child = 10 to 60 meq/24 hours urine (10 to 60 mmol/day)
- Values are diet-dependent.
- Increased urinary K+ is seen in:
- Diabetic and renal tubular acidosis.
- Primary renal diseases.
- Cushing’s syndrome.
- Starvation.
- Primary and secondary aldosteronism.
- Fanconi’s syndrome.
- The onset of metabolic alkalosis.
- The decreased urinary K+ value is seen in:
- Addison’s disease.
- In patients with K+ deficiency.
- Pyelonephritis and glomerulonephritis.
- Indications:
- To evaluate the electrolyte imbalance.
- Renal disorders.
- Adrenal glands disorder.
Macroscopic hematuria:
- It shows cloudy urine with a red to brown color.
- This is seen in:
- Trauma.
- Acute infection.
- Inflammation.
- Coagulation disorders.
Microscopic hematuria is seen in:
- Glomerular diseases.(AGN)
- Malignancy of the urinary tract.
- Renal calculi.
- The possibility of menstrual contamination should be considered in females.
Normal WBCs number:
- Normally few Neutrophils are seen.
- Usually 4 to 5 /HPF.
- >30 cells /HPF is considered an infection.
- WBCs clumps are a sign of infection and must be reported
Increased neutrophils are seen in:
- All renal inflammatory diseases.
- Glomerulonephritis.
- Cystitis and urethritis.
- Chronic pyelonephritis.
- Prostatitis.
- Pyogenic infection.
- Acute appendicitis.
- Acute pancreatitis.
- Tuberculosis.
- Urinary bladder tumors.
Nonbacterial increased WBCs are seen in:
- SLE.
- Interstitial nephritis.
- Glomerulonephritis.
- Tumors.
Epithelial cell found in .....
- Acute tubular necrosis.
- It is seen in heavy metal poisoning.
- Drug-induced toxicity.
- Hemoglobin and myoglobin toxicity.
- Viral infections like HBV.
- Pyelonephritis.
- Viral infections.
- Allergic reactions.
- Acute allogenic Rejection phenomenon.
- Malignant infiltration.
Hyaline casts found ....
- Normally Hyaline casts are seen in :
- After severe exercise.
- Dehydration.
- Emotional stress.
- Heat exposure.
- Pathologically hyaline casts are seen in:
- Acute glomerulonephritis.
- Chronic renal disease.
- Pyelonephritis.
- Congestive heart failure.
- > 20 / PHF is seen in moderate or severe renal disease.
- Granular casts are seen in:
- Acute tubular necrosis.
- Pyelonephritis.
- Advanced glomerulonephritis.
- Malignant nephrosclerosis.
- The increased number indicates severe renal disease.
Red Blood Cell cast Found in.....
- Subacute bacterial endocarditis
- Goodpasture’s syndrome
- Renal infarct
- Acute glomerulonephritis
- Lupus nephritis
- Epithelial cells cast Found in....
- Transplant rejection
- Tubular necrosis
- Heavy metal toxicity
- Salicylates toxicity
- CMV infection