Diseases with ECG change
Protocols
MYOCARDIAL INFARCTION
Before diagnosing myocardial infarction, remember to mention the following points:
• Criteria of infarction (by looking for ST elevation, Q wave, T inversion).
• Site of infarction (whether anterior, inferior, septal, lateral).
• Recent or old.
Sites of Myocardial Infarction is Detected in Different Leads
• Inferior MI — LIII and aVF (may be in LII).
• Extensive anterior MI — V1 to V6.
• Anteroseptal MI — V1 to V3 or V4 (mainly V2 to V4).
• Lateral MI — LI, aVL, V5 and V6.
• Posterior (true) MI — V1 and V2 (may be V1 to V4).
• Subendocardial MI — Symmetrical T inversion in all chest leads (non Q wave MI).
• High lateral — L1 and aVL.
• Anterolateral — L1, aVL, V1 to V6.
• Right ventricular infarction — V3R and V4R.
ECG Criteria of Acute MI (Fully Evolved Case)
• ST elevation (with upward convexity).
• Pathological Q wave.
• T inversion.
ECG Criteria in Old MI
• Pathological Q wave.
• ST—in baseline.
• T—normal or inverted.
According to duration, MI are of 3 types:
• Hyperacute.
• Acute.
• Fully evolved phase.
ECG Criteria in Hyperacute MI (within First Few Minutes)
• ST—slope elevation.
• T—tall, pointed and upright, wide.
• R—increased amplitude.
• Q—absent.
• Ventricular activation time (VAT)—increased.
ECG Criteria in Subendocardial MI (Non-Q Wave MI or Non-ST Elevation)
• T—deeply inverted in chest leads (usually symmetrical T inversion).
• ST—depression.
• Q wave—absent.
ECG Criteria in True Posterior MI
• R—tall and slightly wide in V1 to V2.
• T—upright, tall, wide and symmetrical in V1 to V2.
• ST—depression.
• R/S ratio—in V1 > 1.
What does the pathological Q, ST elevation and T inversion signify in MI?
Ans. As follows:
• Q wave is due to myocardial necrosis.
• ST elevation is due to myocardial injury.
• T inversion is due to ischemia.
LEFT VENTRICULAR HYPERTROPHY
ECG criteria of LVH (voltage criteria):
• S in V1 + R in V6 or V5 > 35 mm (S V1 + R V6 > 35 mm).
(This criteria is applicable only above 25 years of age).
Other criteria of LVH:
• R in V5 (or V6) > 26 mm.
• R in aVL > 11 mm (or 13 mm).
• R in aVF > 20 mm (also in LII and LIII).
• R in LI + S in LIII > 25 mm.
• R in LI > 15 mm.
• R in V6 is equal to or greater than R in V5 (normally R in V5 is taller than R in V6).
• S in V1 or V2 > 25 mm.
• Sum of all QRS in all 12 leads > 175 mm.
• Left axis deviation (QRS between –30° and –90°).
What are the causes of LVH?
Ans. As follows:
• Systemic hypertension.
• Aortic stenosis.
• Coarctation of aorta.
• Hypertrophic cardiomyopathy.
• VSD.
• Mitral regurgitation.
• Aortic regurgitation.
• Patent ductus arteriosus.
• Coronary artery disease (long standing).
RIGHT VENTRICULAR HYPERTROPHY
ECG Criteria
Tall R wave in V1 > 7 mm (also deep S in V5 or V6).
Other Criteria
• R/S ratio in V1 > 1 (R is > S in V1).
• R in V1 + S in V5 or V6 is equal to or > 10.5 mm.
• R in aVR > 5 mm.
• S in V1 < 2 mm.
• Incomplete RBBB (rSR in V1).
• QRS-wide.
• Small q in V1.
• Right axis deviation (between + 90° and + 180°).
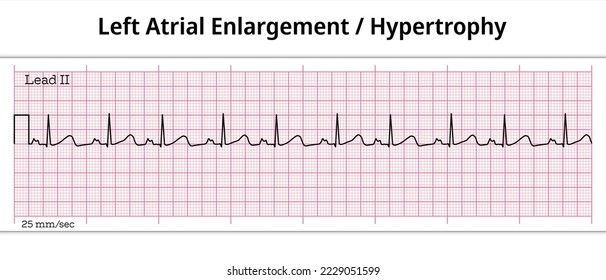
LEFT ATRIAL HYPERTROPHY

ECG Criteria
• P-Wide > 0.12 second (> 2.5 small squares), P may be notched or bifid (like M), called P mitrale (It is better seen in
LII, also in LI and aVL).
• P in V1-Biphasic, with prominent, deep negative deflection (> 1 mm depth) and small initial positive deflection.
RIGHT ATRIAL HYPERTROPHY
ECG Criteria
• P - Tall, > 2.5 mm (> 2.5 small squares), better seen in LII, LIII, aVF and sometimes in V1 (Tall P is called P pulmonale).
• P in V1 - Biphasic, tall initial positive deflection (> 1.5 mm) with a small negative deflection (only positive deflection
may be present).
ATRIAL FIBRILLATION
ECG Criteria
• P wave: Absent (P may be replaced by fibrillary f wave).
• Rhythm: Irregularly irregular (R-R interval is irregular).
(Atrial rate is very high and ventricular rate is less).
According to the rate, atrial fibrillation may be of 2 types:
• Fast atrial fibrillation: Heart rate >100 beats/min.
• Slow atrial fibrillation: Heart rate <100 beats/min.
ATRIAL FLUTTER
ECG Criteria
• P—saw toothed appearance (normal P is replaced by flutter or F wave. Better seen in lead II, III, aVF, and V1).
• RR—regular (may be irregular, when there is variable block).
(Atrial rate—250 to 350 beats /minute, ventricular rate—variable, may be 2:1, 3:1, 4:1, it is then called flutter with
variable block).
NB: Occasionaly, atrial fibrillation and flutter may be present together, it is called flutter fibrillation.
VENTRICULAR ECTOPIC
ECG Criteria
• P—absent.
• QRS—wide > 0.12 second (3 small squares).
• T—opposite to major deflection.
Q. What are the types of ventricular ectopics?
Ans. Ventricular ectopics may be of different types:
• Unifocal: Similar configuration of ectopics in all leads and originates from a single ectopic ventricular focus
(QRS-similar).
• Multifocal: Variable configuration of ectopics in same lead, because ectopics originate from different focus of
ventricle (QRS-variable).
• Interpolated ventricular ectopics: It means when ventricular ectopics occur between two normal sinus beat without
compensatory pause (it is usually associated with sinus bradycardia).
VENTRICULAR TACHYCARDIA
ECG Criteria
• P wave—absent (Dissociated P wave may be seen).
• QRS—broad > 0.14 second, abnormal or bizarre pattern.
• Rate > 100 beats /minute (usually, 140 to 220 beats/min).
Other Criteria
• Occasional capture beat is present (normal sinus P, QRS and T in between ventricular tachycardia).
• Fusion beat (conducted sinus impulse fuses with impulse from tachycardia).
• QRS—in chest leads (V1 to V6) either all positive or all negative (called ventricular concordance).
FIRST-DEGREE AV BLOCK
ECG Criteria
• PR interval—prolonged > 0.22 second (normal 0.12 to 0.20 second).
• QRS—normal.
• Rhythm—normal.
First degree heart block
Q. What are the causes of first degree AV block ?
Ans. As follows:
• Normally in athlete (due to increased vagal tone).
• Drugs (digitalis toxicity).
• Acute myocardial infarction (common in inferior MI).
• Acute rheumatic carditis.
• In elderly (atherosclerosis).
• Hyperkalemia.
Q. What is first degree heart block ?
Ans. It is the simple prolongation of PR > 0.22 sec. Every atrial depolarization is followed by conduction to the
ventricles, but with delay.
SECOND DEGREE AV BLOCK
Second degree AV block may be of 3 types:
• Mobitz type I (Wenckebach’s phenomenon).
• Mobitz type II.
• 2 : 1 or 3 : 1 heart block.
MOBITZ TYPE I (WENCKEBACH’S PHENOMENON)
ECG Criteria
• Progressive lengthening of PR interval followed by absent QRS complex (one P is not followed by a QRS complex).
• PP—constant.
• RR—irregular.
(Progressive shortening of R-R interval until block occurs).
MOBITZ TYPE II AV BLOCK
ECG Criteria
• Some P waves are not followed by QRS complexes.
• PR interval is constant (also PP interval constant).
• QRS—wide.
(In 2 :1 AV block, alternate P wave is conducted. It may be 3:1, 4:1).
This type of AV block is rare and more severe. It is generally a sign of severe conduction system disease.
COMPLETE HEART BLOCK (3RD DEGREE)
ECG Criteria (Rate is Supposed Here)
• Atrial rate—80/minute (PP interval).
• Ventricular rate—35/minute (RR interval).
• PP interval—constant.
• No relationship between P wave and QRS complex (PR looks variable—a clue).
RIGHT BUNDLE BRANCH BLOCK
ECG Criteria
• RSR—in V1 and V2 (M pattern).
• QRS—wide, > 0.12 second (3 small squares).
• Other criteria—broad, deep S in V5 and V6 (also in L1 and aVL).
ECG in incomplete right bundle branch block:
• Same findings as above and QRS is not wide, < 0.12 second.
Q. What are the causes of right bundle branch block?
Ans. As follows:
• Normal variant (common). One percent in young adult and 5% in elderly.
• Coronary artery disease—commonly acute myocardial infarction.
• Atrial septal defect (ASD). Other congenital heart disease—Fallot’s of tetralogy, pulmonary stenosis, VSD.
• Right ventricular hypertrophy.
• Chronic corpulmonale.
• Pulmonary embolism.
• Cardiomyopathy
• Conduction system fibrosis.
LEFT BUNDLE BRANCH BLOCK
ECG Criteria
• RSR’—in V5 and V6, also in LI and aVL (M pattern).
• QRS—wide, > 0.12 second (3 small squares).
(ECG - QRS looks wide from L1 to all leads—A clue for diagnosis).
ACUTE PERICARDITIS
ECG Criteria
• ST—elevated with upward concavity (chair shaped or saddle shaped)—better seen in LI, LII, aVL, aVF, V4 to V6.
• T—upright in acute phase.
Subsequent ECG changes:
• ST returns to baseline.
• T inversion that remains for weeks to months.
WOLFF-PARKINSON-WHITE (WPW) SYNDROME
ECG Criteria
• PR—short < 0.12 second.
• QRS—wide.
• Delta wave—in the upstroke of QRS (slurred QRS).
• Q wave—may be present in lead II, III and aVF (confused with inferior myocardial infarction).
SINUS TACHYCARDIA
ECG Criteria
• Heart rate— > 100 beats/minute.
• P, QRS and T—normal.
• Rhythm—regular.
SINUS BRADYCARDIA
ECG Criteria
• Heart rate— < 60/minute.
• P, QRS and T—normal.
• Rhythm—regular.
SUPRAVENTRICULAR TACHYCARDIA
ECG Criteria
• P—absent.
• QRS—narrow.
• Rhythm—regular.
• Heart rate—high (150 to 250/minute).
DIGITALIS (DIGOXIN) EFFECT
ECG Criteria
• ST—depression (sloping or scooping depression, reverse tick mark, may be rounded concave that looks like thumb
impression, mostly in V4 to V6).
• QT—short.
NB: This effect is not due to digitalis toxicity, rather indicates digoxin effect.
HYPOKALEMIA

ECG Criteria
• U—prominent in chest leads (most common).
• Others—ST depression, T is small or inverted, prolonged PR interval.
Q. What are the effects of hypokalemia on heart?
Ans. As follows:
• Arrhythmia—atrial and ventricular including ventricular tachycardia, ventricular fibrillation.
• Aggravates digoxin toxicity.
• Cardiac arrest (in diastole).
HYPERKALEMIA
ECG Criteria
• T—tall, peaked and tented (in chest leads).
• P—wide, small, ultimately absent.
• PR interval—prolonged.
• QRS—wide, slurred and bizarre.
DEXTROCARDIA
ECG Criteria
• P wave: Inverted in LI, (upright in LIII).
• R wave: Tall in V1, diminishing progressively in V5 and V6.
• Right axis: Deviation.