ECG Basic A-Z
Protocols
DEFINITION
It is the graphical representation of electrical potentials produced when the electric current passes through the heart.
Electrical activity is the basic characteristic of heart and is the stimulus for cardiac contraction. Disturbance of electrical
function is common in heart disease.
Electrocardiogram (ECG) records the electrical impulse on ECG paper by electrodes placed on body surface called
waves or deflections.
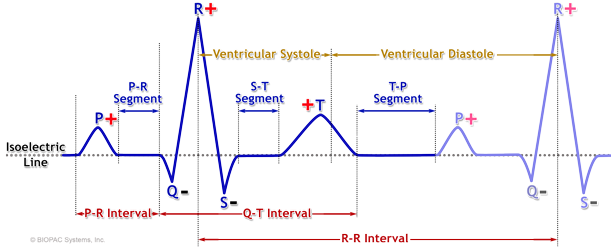
One beat is recorded as a grouping of waves called P-QRS-T.
• P — Represents atrial depolarization.
• PR interval — Represents the time taken for the cardiac impulse to spread over the atrium and through
AV node and His-Purkinje system.
• QRS — Represents ventricular depolarization.
• T wave — Represents ventricular repolarization.
In a normal ECG recording, there are 12 leads:
• 3 bipolar standard leads.
• 3 unipolar limb leads.
• 6 chest leads.
(Leads are different view parts of heart's electrical activity).
1. Bipolar standard leads (also called limb leads) designated as LI, LII and LIII.
• LI — Difference of potential between left arm and right arm (LA and RA).
• LII — Difference of potential between right arm and left leg (RA and LL).
• LIII — Difference of potential between left arm and left leg (LA and LL).
2. Unipolar limb leads (also called augmented limb leads) designated as aVR, aVL and aVF. Three unipolar leads
have very low voltage, which cannot be recorded satisfactorily. For this reason, recordings of these leads are increased
in amplitude. So, they are called augmented unipolar leads, which are represented as aVR, aVL and aVF.
• aVR — Augmented unipolar RA lead. Records the changes of potential occurring in the part of heart facing
towards right shoulder.
• aVL — Augmented unipolar LA lead. Records the changes of potential of heart facing towards the left
shoulder.
• aVF — Augmented unipolar LL lead. Records the changes of potential of heart facing towards the left hip.
3. Chest leads (Unipolar) Designated by 'V'.
Electrodes are placed in the following places on the chest wall.
• V1—4th intercostal space at right sternal border.
• V2—4th intercostal space at left sternal border.
• V3—midway between V2 and V4 lead on left side.
• V4—5th intercostal space in left midclavicular line.
• V5—5th intercostal space in left anterior axillary line.
• V6—5th intercostal space in left midaxillary line.
VIEW OF THE HEART IN ALL LEADS
By looking the following leads, the site and surface of heart lesion is identified.
• LI, aVL, V5 and V6—Reflects lateral (or anterolateral aspect of heart).
• LII, LIII and aVF—Reflects inferior aspect of heart.
• V1 and V2—Reflects right ventricle.
• V3 and V4—Reflects interventricular septum.
• V5 and V6—Reflects left ventricle.
• V1 to V6—Reflects anterior aspect of heart.
• LI, aVL, V1 to V6—Reflects extensive anterior aspect of heart or anterolateral.
• LI and aVL—High lateral.
• LII, LIII, aVF, LI, aVL, V5 and V6—Inferolateral.
INTERPRETATION OF ECG:
Before interpreting an ECG, one must know details about the ECG paper,
standardization and different waves in ECG, etc. It is a matter of experience and pattern
interpretation, which requires a method of systematic ECG analysis.
During interpretation, look at the following points carefully:
1. Standardization (see in the beginning)—like this which is 10 mm (1 mV).
2. Paper speed—25 mm/second.
3. Rhythm—by looking at RR interval (LII is usually called rhythm lead), see regular or irregular.
4. Count the heart rate.
5. Different waves:
• P—whether normal, small or tall, inverted, wide, notched, bifid, variable configuration, etc.
• PR interval—normal or prolonged or short.
• Q—normal or pathological.
• R—normal or tall or short, notched or M pattern.
• QRS—normal or wide, high or low voltage, variable or change of shape.
• ST segment—elevated or depressed.
• T—normal or tall or small or inverted.
• U wave—normal or small.
• QT—short or prolonged.
6. Axis—whether normal or right or left axis deviation.
7. Abnormalities—any arrhythmia, infarction, hypertrophy, etc.
One must have some basic idea about the ECG paper, normal ECG tracing,
limits of normal value, duration, rhythm, etc.
Diseases diagnosed by looking at an ECG:
• Tachycardia or bradycardia.
• Chamber enlargement.
• Myocardial infarction.
• Arrhythmias.
• Block (First degree block, SA block, AV block, bundle branch block).
• Drug effect (such as digoxin).
• Extracardiac abnormalities—electrolyte imbalance (such as hypokalemia or hyperkalemia),
hypo- or hypercalcemia, low voltage tracing (in myxedema, hypothermia, emphysema).
• Exercise ECG to see coronary artery disease.
Standard ECG Paper:
ECG paper shows small and large squares. In each small square, thin horizontal and vertical
lines are present in 1 mm interval. A heavier thick line is present in every 5 mm (5 small squares) interval.
Time is measured horizontally and voltage / height is measured vertically.
1. One small square:
• Height = 1 mm.
• Horizontal (in time) = 0.04 second.
2. One big square (5 small squares):
• Height = 5 mm.
• Horizontal (in time) = 0.04 × 5 sec = 0.2 second.
So, 0.2 second = 5 mm.
1 second = 5/0.2 = 25 mm.
So, recording speed is 25 mm/sec. (i.e. 1500 mm/min).
A faster recording speed (50 mm/sec) is occasionally used to visualize wave deflection.
3. Isoelectric line: It is the base line in ECG paper. Waves are measured either above (positive deflection) or below
(negative deflection).
Standardization of ECG
• Normally, 1mv current — 10 mm height (10 small squares)
• Half strength — 5 mm
• Double strength — 20 mm
• Recording speed — 25 mm/second (i.e. 1500 mm/min)
In any ECG, before telling low voltage or high voltage, see the normal standardization (i.e. 10 mm in height).
![]()
Ref: Devidson medicine
CRITERIA OF LOW VOLTAGE TRACING
• In standard limb leads—QRS < 5 mm (mainly R wave).
• In chest leads—QRS < 10 mm (mainly R wave).
CAUSES OF LOW VOLTAGE ECG TRACING
• Incorrect standardization (i.e. if < 10 mm).
• Obesity.
• Pericardial effusion.
• Chronic constrictive pericarditis.
• Myxedema.
• Emphysema.
• Hypothermia.
ECG CONVENTIONS AND INTERVALS
• Depolarization towards the electrode — Positive deflection (above the isoelectric line).
• Depolarization away from the electrode — Negative deflection (below the isoelectric line).
• Sensitivity — 10 mm = 1 mV.
• Paper speed — 25 mm/second.
• Each large (5 mm) square — 0.2 second.
• Each small (1 mm) square — 0.04 second.
• Normal standardization — 10 mm.
• Rhythm — Interval between two successive R R.
Reference:
1.Ecg in medical practice by AMB Abdullah . 2. Dr.Samol ecg .3.Osmosis Ecg. 4.Oxford ecg
P WAVE
Characters of Normal P Wave
• P wave results from spread of electrical activity through the atria.
• Width or duration (in time, horizontally) - 0.10 sec (2.5 small sq.).
• Height - 2.5 mm (2.5 small sq.).
(Height × Duration = 2.5 × 2.5 small squares).
• P wave is better seen in LII, as atrial depolarization is towards LII (also seen in V1),
because the impulse spread from right to left atrium.
• P wave is upright in all leads, mainly LI, LII and aVF (except aVR). (P is inverted in aVR and occasionally in aVL).
• P wave in V1 may be biphasic (equal upward and downward deflection), notched and wide. (Activation of right
atrium produces positive component and activation of left atrium produces negative component).
• Normal P is rounded, neither peaked nor notched.
Abnormalities of P Wave
P wave may be:
• Absent.
• Tall or small.
• Wide, notched, biphasic.
• Inverted.
• Variable and multiple.
Causes of absent P wave
• Atrial fibrillation (P is absent or replaced by fibrillary f wave).
• Atrial flutter (P is replaced by flutter wave, which shows saw-tooth appearance).
• SA block or sinus arrest.
• Nodal rhythm (usually abnormal, small P wave).
• Ventricular ectopic and ventricular tachycardia.
• Supraventricular tachycardia (P is hidden within QRS, due to tachycardia).
• Hyperkalemia.
• Idioventricular rhythm.
Causes of tall P wave
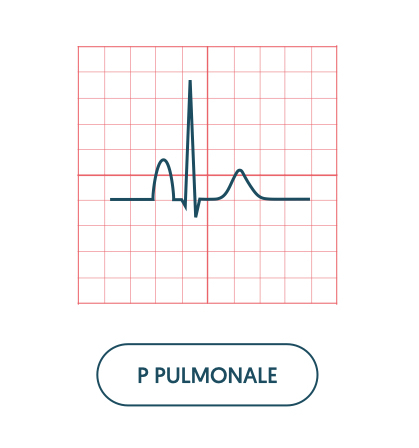
• Tall P is called P pulmonale (height > 2.5 mm, i.e. > 2.5 small squares).
• It is due to right atrial hypertrophy or enlargement.

Causes of small P wave
• Atrial tachycardia.
• Atrial ectopic.
• Nodal rhythm (high nodal).
• Nodal ectopic (high nodal).
Causes of wide P wave
• Broad and notched P is called P mitrale (duration > 0.11 sec, or > 2.5 small squares).
• It is due to left atrial hypertrophy or enlargement.
• In V1, P wave may be biphasic with a small positive wave preceding a deep and broad negative wave (indicates left
atrial enlargement or hypertrophy).
Causes of inverted P wave (negative in LI, LII and aVF)
• Incorrectly placed leads (reversed arm electrodes).
• Dextrocardia.
• Nodal rhythm with retrograde conduction.
• Low atrial and high nodal ectopic beats.

Causes of variable P waves
Presence of variable P waves indicates wandering pacemaker.
Causes of multiple P waves (consecutive 2 or more)
• A-V block (either partial or complete heart block).
• SVT with AV block.
P-R INTERVAL
Characters of Normal P-R Interval
• It is the distance between the onset of P wave to the beginning of Q wave
(if Q wave is absent, then measure up to the onset of R wave).
• It is the time required for the impulse to travel from SA node to the ventricular muscle.
(The impulse is transmitted to ventricle via AV node).
• P-R interval varies with age and heart rate. (P-R interval is short, if the heart rate is increased and long,
if heart rate is decreased).
• Normal PR interval—0.12 to 0.20 sec (maximum 5 small squares).
— In children, upper limit is 0.16 sec.
— In adolescent, upper limit is 0.18 sec.
— In adult, upper limit is 0.22 sec.
• P-R is short, if it is < 0.10 sec and long, if it is > 0.22 sec.
Abnormalities of P-R Interval
PR interval may be:
• Prolonged.
• Short.
• Variable.
Fig: 1st degree A-V block(prolong P-R )
Prolonged P-R interval (> 0.2 second): It is due to first degree heart block. Causes are:
• Ischemic heart disease (occasionally, inferior MI).
• Acute rheumatic carditis.
• Myocarditis (due to any cause).
• Atrial dilatation or hypertrophy.
• Hypokalemia.
• Drugs—digitalis toxicity, quinidine, occasionally β-blocker, calcium channel blocker (verapamil).

Short P-R interval (< 0.12 second): Causes are:
• Wolff-Parkinson-White (WPW) syndrome. In this case, there is delta wave.
• Lown-Ganong-Levine (LGL) syndrome. In this case, there is no delta wave.
• Nodal rhythm.
• Nodal ectopic (high nodal).
• Occasionally, if dissociated beat is present and also in infant, steroid therapy.
Variable P-R interval: Causes are:
• Wenckebach’s phenomenon (Mobitz type I): There is progressive lengthening of P-R interval
followed by a drop beat.
• Partial heart block (Mobitz type II): PR interval is fixed and normal, but sometimes P is not followed by QRS.
• 2 :1 AV block: Alternate P wave is not followed by QRS.
• Complete AV block: No relation between P and QRS.
• Wandering pacemaker: Variable configuration of P.
Q WAVE
Characters of Normal Q Wave
• Q wave is usually absent in most of the leads. However, small q wave may be
present in I, II, aVL, V5 and V6. This is due to septal depolarization.
• Small q may be present in LIII (which disappears with inspiration).
• Depth—< 2 mm (2 small squares).
• Width—1 small square.
• It is 25% or less in amplitude of the following R wave in the same lead.
Characters of Pathological Q Wave
• Deep > 2 mm (2 small squares).
• Wide > 0.04 sec or more (> 1 mm or 1 small square).
• Should be present in more than one lead.
• Associated with loss of height of R wave.
• Q wave should be > 25% of the following R wave of the same lead.
Causes of Pathological Q Wave
• Myocardial infarction (commonest cause).
• Ventricular hypertrophy (left or right).
• Cardiomyopathy.
• LBBB.
• Emphysema (due to axis change or cardiac rotation).
• Q only in LIII is associated with pulmonary embolism (SI, QIII and TIII pattern).
R WAVE
Characters of Normal R Wave
• It is the first positive (upward) deflection, due to ventricular depolarization.
• Duration < 0.01 sec.
• R wave usually small (< 1 mm) in V1 and V2. It increases progressively in
height in V3 to V6 (tall in V5 and V6), i.e. R is small in V1 and V2, tall in V5 and V6.
Normal Height of R Wave
• aVL < 13 mm.
• aVF < 20 mm.
• V5 and V6 < 25 mm.
(If R wave is > 25 mm, it is always pathological).
Abnormalities of R Wave
R wave may be:
• Tall.
• Small.
• Poor progression.
Causes of tall R wave
1. Left ventricular hypertrophy (in V5 or V6 > 25 mm, aVL >13 mm, aVF > 20 mm).
2. In V1, tall R may be due to:
• Normal variant.
• Right ventricular hypertrophy (RVH).
• True posterior myocardial infarction.
• WPW syndrome (type A).
• Right bundle branch block.
• Dextrocardia.
Causes of small R wave: Looks like low voltage tracing.
• Incorrect ECG calibration (standardization).
• Obesity.
• Emphysema.
• Pericardial effusion.
• Hypothyroidism.
• Hypothermia.
R wave progression: The height of R wave gradually increases from V1 to V6.
This phenomenom is called R wave progression.
Poor progression of R wave: Normally, amplitude of R wave is tall in V5 and V6.
In poor R wave progression, amplitude of R wave is progressively reduced in V5 and V6.
Causes are:
• Anterior or anteroseptal myocardial infarction.
• Left bundle branch block.
• Left ventricular hypertrophy (though R is tall in most cases).
• Dextrocardia.
• Cardiomyopathy.
• COPD.
• Left sided pneumothorax.
• Left sided pleural effusion (massive).
• Marked clockwise rotation.
• Chest electrodes placed incorrectly.
• Deformity of the chest wall.
• Normal variation.
S WAVE
Characters of Normal S Wave
• It is the negative deflection after R wave (1/3rd of R wave).
• Normally, deep in V1 and V2 as impulse is going to the muscles of
left ventricle then to the right ventricle.
• Progressively diminished from V1 to V6 (small S wave may be present in V5 and V6).
• In V3, R and S waves are almost equal (corresponds with interventricular septum).
QRS COMPLEX
Characters of Normal QRS Complex
• QRS complex represents depolarization of ventricular muscles.
• Depolarization of left ventricle contributes to main QRS
(as the left ventricle has 2 to 3 times mass of right ventricle).
• QRS is predominantly positive in leads that look at the heart from left side—L1, aVL, V5 and V6.
• It is negative in leads that look at the heart from the right side—aVR, V1 and V2.
• In V1, S is greater than R.
• In V5 and V6, R is tall.
• QRS appears biphasic (part above and part below the base line) in V3 and V4.
• Normal duration of QRS is 0.08 to 0.11 second (< 3 small squares) and height < 25 mm.
Various Forms and Components of QRS Complex
• Q wave: Initial downward deflection.
• R wave: Initial upward deflection.
• S wave: Downward deflection after R wave.
• rS complex: Small initial r wave, followed by large S wave.
• RS complex: A complex with R and S wave of equal amplitude.
• Rs complex: A large R wave followed by a small s wave.
• qRS complex: Small initial downward deflection, followed by a tall R which is followed by a large S.
• Qr complex: Large Q, followed by a small r.
• QS complex: Complex with complete negative deflection (no separate Q and S).
• rSr complex: Small r, then deep S, followed by small r.
• RSR complex: Tall R, then deep S, followed by tall R.
• RR complex: When deflection is completely positive and notched (M pattern).
Abnormalities of QRS Complex
QRS may be:
• High voltage.
• Low voltage.
• Wide.
• Change in shape.
• Variable.
Causes of high voltage QRS
• Incorrect calibration.
• Thin chest wall.
• Ventricular hypertrophy (right or left or both).
• WPW syndrome.
• True posterior myocardial infarction (in V1 and V2).
Causes of low voltage QRS (< 5 mm in LI, LII, LIII and < 10 mm in chest leads)
• Incorrect calibration.
• Thick chest wall or obesity.
• Hypothyroidism.
• Pericardial effusion.
• Emphysema.
• Chronic constrictive pericarditis.
• Hypothermia.
Causes of wide QRS (> 0.12 second, 3 small squares)
• Bundle branch block (LBBB or RBBB).
• Ventricular ectopics.
• Ventricular tachycardia.
• Idioventricular rhythm.
• Ventricular hypertrophy.
• Hyperkalemia.
• WPW syndrome.
• Pacemaker (looks like LBBB with spike).
• Drugs (quinidine, procainamide, phenothiazine, tricyclic antidepressants).
Causes of changes in shape of QRS
• Right or left bundle branch block (slurred or M pattern).
• Ventricular tachycardia.
• Ventricular fibrillation.
• Hyperkalemia.
• WPW syndrome.
Causes of variable QRS
• Multifocal ventricular ectopics.
• Torsades de pointes.
• Ventricular fibrillation.
ST SEGMENT
Characters of Normal ST Segment
• Measured from the end of S to the beginning of T wave. It represents
beginning of ventricular repolarization.
• Normally, it is in isoelectric line (lies at same level of ECG baseline).
• ST elevation is normal up to 1 mm in limb leads and 2 mm in chest leads (mainly V1 to V3).
• In Negroes, ST elevation of 4 mm may be normal, which disappears on exercise.
• Normally, ST segment may be depressed, < 1mm
.
Abnormalities of ST Segment
ST segment may be:
• Elevated.
• Depressed.

Causes of ST elevation (> 2 mm)
• Recent myocardial infarction (ST elevation with convexity upward).
• Acute pericarditis (ST elevation with concavity upward, chair shaped or saddle shaped).
• Prinzmetal’s angina (ST elevation with tall T).
• Ventricular aneurysm (persistent ST elevation).
• Early repolarization (high take off).
• Normal variant in Africans and Asians.
• May be in hyperkalemia.
Causes of ST depression (below the isoelectric line)
• Acute myocardial ischemia (horizontal or down slope ST depression with sharp angle ST-T junction).
• Ventricular hypertrophy with strain (ST depression with convexity upward and asymmetric T inversion).
• Digoxin toxicity (sagging of ST depression—like thumb impression, also called reverse tick).
• Acute true posterior myocardial infarction (in V1 and V2), associated with dominant R and tall upright T wave.
Early repolarization (high take-off)
• It is a benign, normal finding in young healthy person, more in black males.
• It is seen in chest leads, commonly V4 to V6 (rarely, in other chest lead).
• ST elevation is usually associated with J point elevation.
• It is not associated with inversion of T wave or abnormal Q wave.
T WAVE
Characters of Normal T Wave
• It indicates ventricular repolarization.
• Follows S wave and ST segment.
• Upright in all leads, except aVR.
• Usually, more than 2 mm in height.
• May be normally inverted in V1 and V2.
• Normally, not more than 5 mm in standard leads and 10 mm in chest leads.
• Minimum 1/4th of R wave of the same lead.
• Tip of T is smooth (rounded).

Abnormalities of T Wave
T wave may be:
• Inverted.
• Tall peaked, tented.
Causes of T inversion
• Myocardial ischemia and infarction.
• Subendocardial myocardial infarction (non-Q wave myocardial infarction).
• Ventricular ectopics.
• Ventricular hypertrophy with strain.
• Acute pericarditis.
• Cardiomyopathy.
• Myxoedema.
• Bundle branch block.
• Drugs (digitalis, emetine, phenothiazine).
• Physiological (smoking, anxiety, anorexia, exercise, after meal or glucose).

Causes of Tall peaked T wave
• Hyperkalemia (tall, tented or peaked).
• Hyperacute myocardial infarction (tall T wave).
• Acute true posterior myocardial infarction (tall T in V1 to V2).
• May be normal in some Africans and Asians.
Causes of Small T wave
• Hypokalemia.
• Hypothyroidism.
• Pericardial effusion.
QT INTERVAL
Characters of Normal QT Interval
• It is the distance from the beginning of Q wave (or R wave, if there is no Q wave) to the end of T wave. It represents
the total time required for both depolarization and repolarization of the ventricles.
• Normal QT interval is 0.35 to 0.43 seconds.
• Its duration varies with heart rate, becoming shorter as the heart rate increases and longer as the heart rate decreases.
In general, QT interval at heart rate between 60 to 90/minute does not exceed in duration half the preceding RR
interval.
• It is better seen in aVL (because there is no U wave).
• Corrected formula for real QT is:
QTC = QT / √ RR
Abnormalities of QT Interval
QT interval may be:
• Short.
• Long.
Causes of short QT interval
• Digoxin effect.
• Hypercalcemia.
• Hyperthermia.
• Tachycardia
Causes of long QT interval
• Hypocalcemia.
• Bradycardia.
• Acute myocarditis.
• Acute myocardial infarction.
• Hypothermia.
• Drug (quinidine, procainamide, flecainide, amiodarone, tricyclic antidepressant, disopyramide, pentamidine).
• Cerebral injury (head injury, intracerebral hemorrhage).
• Hypertrophic cardiomyopathy.
• During sleep.
• Hereditary syndrome:
(a) Jervell-Lange Nielsen syndrome (congenital deafness, syncope and sudden death).
(b) Romano-Ward syndrome (same as above except deafness).
